By Jennifer Avery
Currently, we only have a little advice when it comes to coding procedures using ICD-9-CM volume 3 codes and most of that comes from AHA Coding Clinic. So I was really excited to see that the cooperating parties developed guidelines with the new ICD-10-PCS system. However, once I began studying them, I noticed some guidelines that are going to cause a challenge for coders since many of these guidelines will change how coders report inpatient procedures using ICD-10-PCS codes. It will also change how coders report procedures using the CPT ® and HCPCS Level II codes for outpatient facility/physician services. So, the ICD-10-PCS draft guidelines bring up a lot of questions as to why the rules will change for the coding of certain procedures using ICD-10-PCS.
The multiple procedure guidelines present possibilities for coder confusion. Several guidelines relate to the coding of multiple procedures, some under the heading of multiple procedures and others dispersed throughout the various root operation guidelines.
In ICD-10-PCS, multiple procedure coding guidelines identify when it is appropriate to report than one procedure code, such as:
- Same root operation is performed on different body parts as defined by distinct values of the body part character
- Same root operation is repeated at different body sites that are not included in the same body part value
- Multiple root operations with distinct objectives are performed on the same body part
- The intended root operation is attempted using one approach, but is converted to a different approach
I would like to take the time to explore each of these concepts individually and identify examples of how coders should apply the guideline, and also, areas where coders face potential issues with application of the guidelines. I will also discuss guidelines that appear to be related to multiple procedures, but are not designated as multiple procedure guidelines.
Building an ICD-10-PCS code
First, let's talk about multiple procedure codes being reported when the same root operation is performed on different body parts as defined by distinct values of the body parts characters. To help understand the guideline, you have to be familiar with the unique structure of the ICD-10-PCS system. Coders build an ICD-10-PCS code by using a "table" format that will allow them to construct multiple codes from a single table. In some cases, coders can construct more than 200 possible codes from a single table.
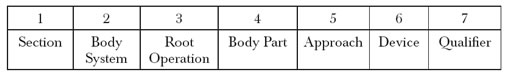
Within the various sections of ICD-10-PCS, each character of the seven-character alphanumeric code identifies "specific" or "general" values. For example, in the Medical & Surgical section, the code is comprised of the following characters:
In the Medical &Surgical section, if separate body part (character 4) values exist, then coders must report multiple codes.
For example, if a physician performed an open total abdominal hysterectomy (removing both the uterus and the cervix), how would the service be reported using ICD-10-PCS codes? By root operation definition, we would look at Resection in the alphabetic index which means "Cutting out or off, without replacement, all of a body part." This leads us to table 0UT- :
0 Medical and Surgical
U Female Reproductive System
T Resection
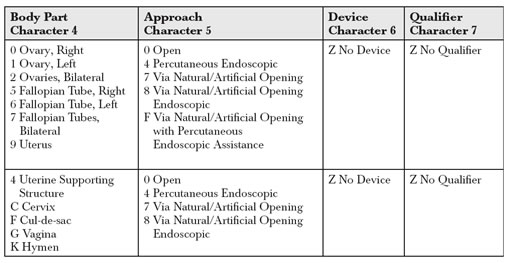
As you can see from the chart, character 4 contains "separate" character values for the uterus (9) and the cervix (C). Therefore, in order to report the procedure, we would need to report two codes: 0UT90ZZ and 0UTC0ZZ. Also, as evident from the table, if the tubes and ovaries were also removed, we would be reporting even more codes for this procedure.
Reporting for similar procedures performed on different body sites
Multiple procedures can also be reported if the same root operation is repeated at different body sites that are included in the same body part value. For example, if a surgeon repairs a torn right posterior cruciate ligament (PCL) and a right lateral collateral ligament (LCL) by open approach during the same operative session, per the body part key, these are both coded to the body part of Knee Bursa and Ligament. However, they are not the same "site" and therefore coders must report the procedure code twice to identify "two" sites were repaired:
0MQN0ZZ for the right PCL repair
0MQN0ZZ for the right LCL repair
I can see a potential problem from a payer's perspective and from a statistical standpoint with the application of this guideline. How do we know they really repaired two separate sites and that it isn't just a clerical error in reporting?
In CPT, we have modifiers that identify right (-RT), left (-LT), bilateral (-50), multiple procedures (-51), and distinct procedures (-59). However, ICD-10-PCS currently does not include anything that would help to identify that these are actually "two" sites.
I believe that I have come up with an easy solution for this one. What about using the qualifier (character 7) to represent the specific different ligaments, etc. in these situations? In many instances, ICD-10-PCS does not define character 7 and therefore adding some type of clarifying information could be a possible option. I guess it will depend on how often this would cause confusion for payers or statistical data gathering.
Reporting for multiple operations on the same body part
Multiple procedures can also be reported during the same operative session when the physician performs multiple root operations with distinct objectives on the same body part.
For example, the physician performs an open partial descending colon resection with enterolysis of large intestinal adhesions. Coders would report both 0DBM0ZZ for Excision of the descending colon and 0DNE0ZZ for Release of the large intestines. Coders report enterolysis of intestinal adhesions with the root operation "Release" for freeing a body part.
So if we also performed another procedure in the abdomen (e.g., resection of the intestines), then it appears as if we can now report both. I believe that this is another multiple procedure guideline that is going to often require clarification either by AHA Coding Clinic for ICD-10 or additional guideline clarification.
Currently, enterolysis of adhesions is considered a part of the procedure unless the physician identifies that the adhesions unusually complicated the procedure in some way. However, based on the ICD-10-PCS guidelines, it appears as if we would be able to report them separately. I believe that we will see more on this in the near future: Is the enterolysis really being performed to "free the body part" or is it an integral part of the more definitive procedure (e.g. Resection)?
What about an ansatomosis after a colon resection? Currently in ICD-9-CM, we only report the anastomosis separately if it is "other than end to end."
In ICD-10-PCS, coders report an anastomosis using root operation "Bypass" for altering the route of passage of the contents of a tubular body part and a colon resection using either root operation "Excision" for removal of a portion of a body part, or "Resection" for removal of all of a body part without replacement. A note in the Introduction to ICD-10-PCS in the OptumInsight (formerly Ingenix) CD-10-PCS manual states that the term anastomosis is not a root operation because it is a means of joining and is always an integral part of another procedure (Bypass, Resection) with a specific objective. However, if you look up anastomosis in the alphabetic index in ICD-10-PCS, it refers you to "Bypass."
This is very confusing. First of all, where does the information in the introduction originate? Is it an official governmental file like the official coding guidelines, or does the introduction come from the various vendors who produce the manuals? Can we assume that the same rules apply in ICD-10-PCS? I for one am not comfortable making assumptions and would like clarification from an authoritative source.
Reporting for procedures that begin with one approach but are converted to another
One multiple procedure guideline caught me off guard. If during the same operative session, the intended root operation is attempted using one approach but is converted to a different approach, coders report multiple codes. This is going to take many of us by surprise and we'll need some time to get comfortable using it.
The example ICD-10-PCS uses is one that we all know. We attempt a laparoscopic cholecystectomy and have to convert it to open. In ICD-10-PCS, you will report the open "Resection" of the gallbladder and also report a laparoscopic "Inspection" of the gallbladder.
This goes against how we code currently in both the inpatient and outpatient settings. We have a coding rule that says, "When you begin laparoscopic and convert to open, you only code the open procedure." We even have an ICD-9-CM diagnosis code that we use as an additional code to identify that a laparoscopic procedure has been converted to open (V64.41).
Well, hang on to your hats, folks, because ICD-10-CM does not include an equivalent to this diagnosis code. Therefore both inpatient and outpatient coders need to be made aware of this guideline because it will change how we report the services. As far as I know, the rule isn't changing for the outpatient facility or physician reporting as far as the procedure. However, once we transition to ICD-10-CM, outpatient coders will no longer have an additional diagnosis code that reflects the true picture of the service(s) performed.
I thought the guideline was pretty clear cut as how to report the services (a code for the Inspection of the gallbladder and a code for the Resection of the gallbladder). I guess the example helped as well for me.
However, a student in an ICD-10 boot camp I was teaching pointed out that they were confused by the wording in the guideline, which creates confusion about what specific procedures to code. Many interpret the guideline to state you would report both a laparoscopic "Resection" of the gallbladder and an open "Resection" of the gallbladder since it says "attempted." Maybe they need to reword the guideline to be more clear-cut. In teaching the guideline, I currently point to the example to clarify what the guidelines mean.
Reporting inpatient facility services vs. outpatient facility/physician services
Other ICD-10-PCS Draft Coding Guidelines are not designated as multiple procedure guidelines, but seem to fall in that category. One of those guidelines happens to fall under the heading of Inspection procedures in the guidelines.
When both an "Inspection" procedure and another procedure are performed on the same body part during the same operative session-if the "Inspection" procedure is performed using a different approach than the other procedure- then coders report the "Inspection" procedure separately.
For example, the physician performed a diagnostic esophagogastroduodenoscopy (EGD) and an open excision of a duodenal lesion during the same operative session. We would report Inspection of the upper intestinal tract (0DJ08ZZ), and the Excision of the duodenum (0DB90ZZ). This may also take some getting used to; does the phrase "diagnostic is always included in therapeutic" come to mind?
Another such guideline falls under the heading of Biopsy followed by more definitive procedure. This one also surprised me. If a diagnostic Excision, Extraction, or Drainage procedure (biopsy) is followed by a more definitive procedure-such as Destruction, Excision, or Resection at the same procedure site- then both the biopsy and the more definitive treatment are coded.
This goes against how we currently code for both inpatient and outpatient services. Currently, if we biopsy a lesion and remove the same lesion, we only code the removal.
It would appear with this guideline that when we move to ICD-10-PCS, we will be coding differently for inpatient services and for outpatient facility/professional services here as well. So, in the inpatient setting, if we would perform an excisional biopsy of the left breast followed by a mastectomy of the left breast, we would code both the Excision of the breast and the Resection of the breast.
My question is whether we get to assume that the Excision of the breast (excisional biopsy) was diagnostic for the correct qualifier (character 7) or does the physician have to specifically identify that the biopsy was diagnostic?
Under the heading of Excision for graft, another multiple procedure guideline identifies that if an autograft is obtained from a different body part in order to complete the objective of the procedure, report the Excision separately. Whoa! So, think about this example: If a surgeon harvested a piece of the left greater saphenous vein for use in an aortocoronary artery bypass of the left anterior descending artery to the aorta, we would report not only the Bypass procedure (021009W), but also the Excision of the saphenous vein (06BQ0ZZ).
This is yet another disconnect between how we will be reporting inpatient facility services and outpatient facility/physician services. We have another rule that we currently follow that says harvesting the saphenous vein is considered a part of the procedure and therefore is not reported separately.
Other multiple procedure guideline examples
Since we are discussing coronary artery bypass procedures, we need to look at another multiple procedure guideline under the heading of Bypass procedures. This guideline states that if the physician bypasses multiple coronary sites, coders report a separate procedure for each coronary artery site that uses a different device and/or qualifier.
We already code this way, so we should have no problem with the guidelines, but actually coding them out is another thing all together. You may have to stop and think when coding these based on the table.
For example, if we performed an aortocoronary artery bypass using a piece of a vein (autograft) to two coronary artery sites (left anterior descending and left circumflex) and also performed a left internal mammary artery bypass, we would report 02100A9 for the LIMA, and 021109W for the two coronary artery sites that were bypassed to the aorta using a vein graft. We actually bypassed three sites based on the body part character that includes when multiple arteries are "Bypassed" using the same device/qualifier.
When it comes to Fusion (e.g. arthrodesis) procedures for the spine, a series of guidelines appear to fit under the heading of multiple procedures. If multiple vertebral joints are fused, a separate procedure is reported for each vertebral joint that uses a different device and/or qualifier. For example, if a surgeon performed an open arthrodesis of T4-5 posterior approach, anterior column with interbody fusion device, and an arthrodesis of T6-7 posterior approach, posterior column with interbody fusion device, you would report two procedure codes: 0RG60AJ and 0RG60A1.
The guideline goes on to identify a sort of hierarchy when it comes to combinations of devices/materials used to fuse the same vertebral joint.
If an interbody fusion device is used to render the joint immobile (either alone or containing other material like bone graft), then code the procedure to the device value for interbody fusion device.
If the physician uses only a bone graft to render the joint immobile, code the procedure with the device value nonautologous tissue substitute or autologous tissue substitute depending on the type of graft.
If the physician renders the joint immobile using a mixture of autologous and nonautologous bone graft (with or without biological or synthetic extenders or binders), code the procedure with the device value autologous tissue substitute.
None of these should come as a big surprise, but we may need some time to get back up to speed with our procedures. They make you stop and think. I find visuals help, a lot.
Bilateral procedure guidelines seem to fit under the heading of multiple procedures guidelines for obvious reasons. At times we will need to report multiple procedures, just as we currently do in both CPT and ICD-9-CM volume 3.
In ICD-10-PCS, if no bilateral body part value exists to report the procedure, coders report each procedure separately using the appropriate body part value. For example, if a surgeon performed bilateral total knee arthroplasty, synthetic joint, cemented, we would report 0SRD0J9 for the left knee and 0SRC0J9 for the right knee. Unlike ICD-9-CM volume 3 codes, ICD-10-PCS identifies the laterality of the procedure.
Conclusion
Besides those discussed above, I have identified a few potential issues when it comes to the practical application of ICD-10-PCS where currently we have more questions than answers.
First, we currently have guidance that defines the principal procedure that would help to identify sequencing in some instances. However, I have not seen anything official addressing sequencing issues in ICD-10-PCS. Those who currently work in inpatient settings understand the importance of getting the principal procedure correct as it could impact financially based on surgical MS-DRGs.
Currently, I assume that the definition of principal procedure isn't going to change and that this will eventually be added to the ICD-10-PCS Manual. However, I would feel better about having it already as a part of the guidelines if it isn't changing.
Another challenge is that oftentimes, certain procedures may appear to fit the definition of more than one root operation and we have the challenge of determining which one.
I highly encourage everyone to begin learning and working with ICD-10-PCS as soon as possible to help identify some of the potential issues when it comes to implementation and practical use. Some further guidance may be added to the code sets and/or the ICD-10-PCS Official Coding Guidelines, or be better addressed by AHA Coding Clinics for ICD-10.
We may also face documentation issues that we never faced before because ICD-9-CM volume 3 codes have always been sort of general. Based on the added specificity required with some code sets in ICD-10-PCS, we may for the first time need to query physicians on certain procedures, which will be a new concept for coders, documentation specialists, and physicians alike. Since we are faced with yet another delay in the implementation, I think we should take advantage of the time and make ICD-10-PCS an even better system than it is. Personally, I think it's pretty great!
Jennifer Avery, CCS, CPC-H, CPC, CPC-I , a senior regulatory specialist with HCPro, Inc., and serves as a lead instructor for the Certified Coder Boot Camp®, the Certified Coder Boot Camp®-Online Version, the Certified Coder Boot Camp®-Inpatient Version, and HCPro's ICD-10 Basics Boot Camp®. As a member of the Revenue Cycle Institute, Avery works with hospitals, medical practices, and other healthcare providers on a wide range of coding-related issues with a particular focus on coding education.

