Modifier 33 was added by the American Medical Association (AMA), and announced at the annual CPT Symposium with an effective date of January 1, 2011. Additional information has been made available during the year.
Modifier 33, Preventive Service: When the primary purpose of the service is the delivery of an evidence-based service in accordance with a US Preventive Services Task Force A or B rating in effect and other preventive services identified in preventive services mandates (legislative or regulatory), the service may be identified by appending modifier 33 Preventive Service, to the service. For separately reported services, even those specifically identified as preventive, the modifier should not be used.
A significant portion of the Patient Protection and Affordable Care Act (PPACA) requires coverage of preventive services and immunizations by insurance payers without a cost sharing provision. These services include those rated as A or B by the US Preventive Services Task Force (USPSTF). This rating is updated at least annually and can be found on the USPSTF website.
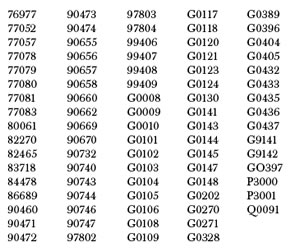
According to the PPACA these A and B services must be provided without co-pay, coinsurance or deductible. Below you will find a listing of those CPT procedure codes identified by the AMA as meeting the criteria for an A or B service as rated by the USPSTF.
If the primary purpose of the visit is to perform these preventive services there is no cost sharing for the A and B services or associated office visit. However, if the primary purpose of the visit is not for the A and B services a cost share may be applied to the office visit component.
It is also important to note that patients receiving A and B services "out of network" may be required to share the cost in whole (non-covered) or part (co-pay, coinsurance, or deductible) as deemed by the payer.
By appending the modifier 33 to the A, B, and encounter service, the provider is indicating that these services meet the USPSTF criteria and should not be subject to cost sharing. The services reported with modifier 33 must be deemed an A or B service by the USPSTF and additional services provided during the same encounter that do not meet the guidelines are subject to cost sharing.
Julie Orton Van, CPC, CPC-P, CEMC, CGSC, COBGC, works at Ingenix as a product manager. She has nearly 30 years experience in the health care industry, including physician office management, home health and hospice, managed care, laboratory services, physician and facility contracting, benefits administration, claims payment, and clinical information systems. Prior to her position at Ingenix, she was a systems analyst for a fully integrated electronic medical record at a large teaching hospital and healthcare system. She can be reached at Julie.Van@Ingenix.com.

