It is a busy time for healthcare providers, and lots of industry changes are redefining how organizations do business. In the past several years, the government has offered incentive programs through The Centers of Medicare and Medicaid Services (CMS) to encourage healthcare providers to adopt certain clinical practices and/or tools: the Physicians Quality Reporting System (PQRS), Electronic Prescribing (eRx), and Electronic Health Records (EHRs), to name a few. The incentive programs use a carrot and stick approach - early adopters or participants can receive additional reimbursement for certain services, but all providers face reduced payments if they fail to adopt the incentive program practices by their respective compliance dates.
In the near future, one change will be imposed on the healthcare industry as a do-or-die approach - the replacement of the ICD-9 code set with ICD-10. On October 1, 2013, providers must report the ICD-10 diagnosis codes on all claims or face denials for their services. With the ICD-10 implementation, there are no incentive payments for early adopters, no grace period for late comers, no reduced fee schedules for claims submitted with ICD-9 codes after the implementation date, and no opportunities to opt out. Healthcare providers must comply, or get out of the healthcare business.
Understandably, many providers are focused on getting their incentive dollars from the PQRS, eRx, and EHR incentive programs, and view ICD-10 as a distant threat that they can worry about later. Others are starting to realize they cannot put off planning for ICD-10 much longer, yet are at a loss as to where to begin.
This article focuses on the preliminary planning stages of the ICD-10 implementation process and the activities in which healthcare providers should currently be engaged.
5010 Transaction Set
On January 1, 2012, the 5010 Transaction Set will replace the existing 4010 Transaction Set used to process claims today. The 5010 conversion will affect all HIPAA covered entities, such as providers, health plans, clearinghouses, and some software vendors. 5010 is designed to reduce transaction costs, minimize manual processing, and introduce new functionality. It will establish the platform needed to report ICD-10 codes in 2013.
Practice administrators should proactively contact their software vendors to see what upgrades are necessary to adapt their systems to the 5010 Transaction Set. For most, the 5010 upgrade will be handled on the back end of the practice management (PM) system, and will have little to no direct impact on physicians. Administrative, coding and billing personnel will be affected the most by the change, and may face a small to moderate learning curve with the new system.
Lastly, administrators should develop a full, end-to-end testing strategy for all internal and external data transactions their practice conducts between HIPAA entities (from provider to PM system to clearinghouse to payer). The 5010 testing should take place at least six to eight weeks prior to January 1, 2012.
Code Freeze
In September 2010, the ICD-9-CM Coordination and Maintenance Committee announced that it will suspend regular updates to the ICD code sets in 2012 and 2013. However, limited updates for new technologies and diseases will still be made to both ICD-9 and ICD-10. The purpose of the partial code freeze is to allow organizations to focus on the ICD-10 conversion without having to manage major revisions to ICD-9, or sabotage any work the organization may have done in the ICD-10 code set prior to the live date. The timeline for the code freeze is as follows:
· October 1, 2011 - Regular, annual updates to both ICD-9 and ICD-10
· October 1, 2012 - Limited updates to both ICD-9 and ICD-10 for new technologies and diseases
· October 1, 2013 - Limited updates to ICD-10 for new technologies and diseases
· October 1, 2014 - Regular, annual updates to ICD-10
ICD-10 Planning
ICD-10 implementation planning will most likely involve two distinct phases. Phase 1 involves important preliminary planning that will lay the foundation for the day-to-day business processes. Phase 1 planning includes creating an ICD-10 implementation team, reviewing business contracts, and upgrading computer systems and applications to enable billing under the ICD-10 code set. Phase 1 activities should take place in 2011 and 2012. By 2013, an organization should be fully involved in phase 2 activities. Phase 2 activities will include testing software applications in the new code set, reformatting charge capture tools (for example, superbills, EHR templates, lab forms), and in-depth code training.
Phase 1 of ICD-10 implementation planning should include the following steps:
1. Establish an ICD-10 team
2. Educate the ICD-10 team members
3. Conduct an impact analysis
4. Create a budget
5. Establish an implementation timeline
ICD-10 Team
A key factor to a successful ICD-10 implementation is having the right people on the job. The ICD-10 team should include employees such as the practice administrator, IT personnel, the coding and/or billing supervisor, the chief financial officer, providers, and other senior management. The mix of team members should cover all major business practices within an organization. From these individuals, the team ought to select a team leader who will direct communications between team members, and when appropriate, staff members outside of the ICD-10 team. Regular communication between team members will be an important part of staying on track with implementation activities.

ICD-10 Team Education
Once the ICD-10 team is established, it is important that all the team members possess a basic knowledge of what ICD-10 is, and a broad view of how it will affect the healthcare industry. It is very possible, even likely, that there will be team members who have no idea what ICD-10 is or how it will affect their departments. The purpose of the ICD-10 education meetings is to get everyone on the same page. Team education should be done very early in the implementation planning, and can likely be achieved in one or two sessions. Once the education sessions have been accomplished, it will help the team to focus more clearly on the next step of the ICD-10 planning - the impact analysis.
Impact Analysis
In early to mid-2011, the ICD-10 team ought to conduct an impact analysis that identifies all areas within the organization that will be affected by the ICD-10 conversion. The impact analysis should cover clinical areas, IT systems, documentation, health plans, employee training, vendor relationships, and more. The impact analysis will also help to identify and define the responsibilities the team members will have during the implementation process.
Administrative
Administrative personnel will mostly be responsible for communicating with business partners outside of the organization, such as software vendors, payers, and clearinghouses. Administrative personnel will be responsible for handling any contract negotiations that may be necessary, as well as, making any financial decisions with regards to software purchases or upgrades. Lastly, it will most likely be these team members who schedule any upgrades with software vendors and coordinate testing between partners.
Information Technology
The IT members of the ICD-10 planning team will be responsible for making sure the technical aspects of the ICD-10 upgrade goes smoothly. Their responsibilities will involve coordinating the upgrades with vendors, trouble shooting system problems, and providing any necessary hardware upgrades within the organization.
Coders, Billers, Providers
Coders, billers and providers are the individuals who will actually be handling ICD-10 codes on a daily basis. As such, they will have a greater need to understand the "method behind the madness," so to speak. ICD-10 code training should cover the following areas:
· Details on the ICD-10 code structure and basic differences from ICD-9
· Instructions on how to use the ICD-10 manual and coding conventions
· Documentation training
· Coding practice sessions
Preliminary training can be done at any time, and there are several resources already available on the market. However, in-depth code training really should not begin until May or June of 2013. If providers begin code training too early, they run the risk of forgetting everything they have learned by the time October 2013 rolls around. In the months leading up to October 1, 2013, it is also a good idea for coders, billers and providers to meet regularly to practice coding encounters in ICD-10. These exercises will help individuals gain familiarity and speed under the new coding system.
In addition, any forms, EHR templates or charge capture tools must be reformatted using the ICD-10 codes. Allow six to nine months to revise or develop these tools, and include practice sessions with the new forms or templates for the providers to weed out any errors or problems.
Create a budget
The impact analysis will help identify financial needs for the ICD-10 conversion. The budget should include funds for ICD-10 code training for coders, billers, and providers. The budget must also include funds for staff overtime, new employees, new hardware, and software upgrades of existing applications. Lastly, it is advisable to create a six to twelve month savings cushion in case there is a disruption to cash flow after the implementation date.
To get an idea of what the ICD-10 conversion will cost, the Nachimson Advisory Study provides the following estimates in Table 1:
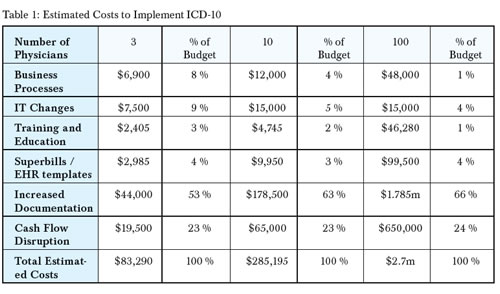
Note: For more details on the Nachimson Advisory Study, go to http://www.aaos.org/news/aaosnow/feb09/reimbursement1.asp.
Timeline
The impact analysis and budget will help the ICD-team formulate an implementation timeline. The timeline ought to identify clear benchmarks to track the organization's progress. When necessary, the timeline may need to be adjusted to accommodate unexpected problems or developments. The timeline will be an important communication tool for the ICD-10 team leader when coordinating between team members and communicating with non-team members in the organization.
In addition, if you are planning to implement an EHR or new PM system in the near future, you should factor these implementations into the ICD-10 timeline. It is advisable that you do not implement anything six months prior to the ICD-10 implementation date. ICD-10 will be overwhelming enough without employees having to navigate the hassles of a new EHR or PM system. The key to survival is good planning!
Conclusion
Major changes are coming to the healthcare industry and organizations cannot afford to sit back and tackle these changes as they come. Organizations must be proactive and strategic in their ICD-10 planning to achieve a smooth transition. Healthcare professionals must be prepared to be flexible and adapt over the coming months. A lot is changing, and no one knows all of the answers. The sooner organizations start ICD-10 planning, the less overwhelming the change will be in the long run.
Resources
ICD-10 Implementation Information
http://www.cms.gov/MLNMattersArticles/downloads/SE1019.pdf
AAPC ICD-10 Implémentation
http://www.aapc.com/ICD-10/
AHIMA Preparing for ICD-10
http://www.ahima.org/icd10/preparing.aspx
AAFP Sample Transition Plan
http://www.aafp.org/online/etc/medialib/aafp_org/documents/prac_mgt/codingresources/transitionicd10.Par.0001.File.tmp/transitionicd10.pdf
ICD-10-CM Quick Reference Guide
http://www.cms.gov/ICD10/Downloads/ICD-10QuickRefer.pdf
AHIMA Top 10 List of Phase I Activities
http://library.ahima.org/xpedio/groups/public/documents/ahima/bok1_048748.pdf
5010 Update: Benefits of Implementation
http://news.aapc.com/index.php/2010/01/5010-update-benefits-of-implementation//
Code Freezing Coming for ICD-9 and 10
http://journal.ahima.org/2010/09/15/code-freeze-coming-for-icd-9-and-10/
Nachimson Advisory Study
http://www.aaos.org/news/aaosnow/feb09/reimbursement1.asp.
Since 2002, Allison Singer, CPC, CPMA has been an employee at White Plume Technologies � a software company that specializes in automated charge capture and code scrubbing solutions. Allison began her career designing encounter forms for over 30 different medical specialties. In 2009, Allison joined the ranks of certified professional coders, launching her career as a medical coding consultant.

