The 2008 interim and final rule with comment period for the Medicare hospital outpatient prospective payment system (OPPS) weighs in at 1,969 pages! As you might imagine, it is chock full of changes to implement new statutory requirements and refine various parts of the payment system. All changes, unless otherwise noted, take effect on January 1, 2008.
Within this tomb of regulations, there are several topics of importance to pharmacy directors, which are summarized below. It is imperative that pharmacy directors possess a solid understanding of these rules. (See Information Source below for sections of the final rule that relate to pharmaceuticals.)
Pharmacy Overhead Costs
To the collective relief of all hospital pharmacy managers, the Centers for Medicare & Medicaid Services (CMS) did not finalize its proposal to require pharmacy departments to remove the overhead charge from the charge of each drug or biological. CMS had proposed that special HCPCS codes be placed on an uncoded revenue line on each Medicare claim.
CMS received many comments stating that this requirement would create an administrative burden for hospitals. Therefore, in the final rule, it backed off on its proposal, which means that no separate accounting of overhead costs for pharmaceuticals and biologics will be required.
Packaging Threshold-and Exemption
In 2008, payment will be packaged for drugs, therapeutic radiopharmaceuticals and biologicals with a median cost per day that is less than or equal to $60-an increase from $55 in 2007. Payment for these pharmaceuticals will be bundled with their associated procedure or treatment and will not be separately payable.
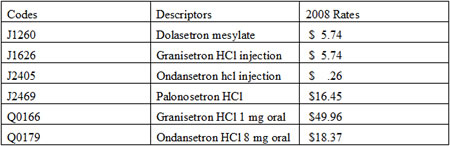
However, in 2008, CMS will continue to exempt one class of anti-emetics, the 5-HT3 receptor antagonists, from the packaging threshold requirement and, instead, will pay for them separately. Table 1 outlines the applicable drugs and their codes.
Table 1: 5-HT3 Exempt From 2008 Packaging
Separately Payable, Non-Pass-Through Drugs
Previously, CMS used only the pricing information for drugs, biologics, and radiopharmaceuticals supplied by manufacturers to calculate reimbursement for hospital OPPS drugs. Recently, the agency announced a plan to begin a transition towards using only mean costs from hospital claims data as a basis for calculating the relative average sales price (ASP) for these drugs. As part of this transition, for 2008, the hospital OPPS payment for separately payable non-pass-through drugs will decrease to ASP + 5 percent in 2008 from ASP + 6 percent in 2007.
However, for pharmaceuticals administered in physicians' offices, CMS will continue to use manufacturer-supplied price data to calculate ASP as the basis for payment. As you may remember from a previous newsletter article, in 2007, CMS reimbursed physicians at the same rate as hospital outpatient departments. For 2008, it finalized its proposal to continue this practice, and pharmaceuticals administered in a physician's office will be reimbursed at a rate of ASP + 6 percent (instead of the ASP + 5 percent for hospital pharmacy departments).
Pass-Through Status-Coming and Going
CMS grants pass-through status to certain "new" and expensive drugs and also pays for them separately while the agency collects sufficient claims data to set payments. In addition, the drug's manufacturer must submit a written request for pass-through status to be granted. Reimbursement for pass-through drugs in 2008 will be paid at a rate of ASP + 6 percent. A drug cannot receive pass-through payment for more than three years. Accordingly, the drugs listed in Table 3 will no longer receive pass-through payments as of January 1, 2008, but will be paid at a reduced rate of ASP + 5 percent.
At the present time, there are no radiopharmaceuticals with pass-through status in 2008. If any are granted this status in 2008, payment would be based on the ASP methodology. Because ASP data are not available for radiopharmaceuticals, CMS will base the pass-through payment on the product's wholesale acquisition cost (WAC) WAC. If that data are also not available, it will then provide payment for the pass-through radiopharmaceutical at 95 percent of its most recent AWP.
Table 2: Pass-Through Status in 2008
As you can see, some codes for the drugs and biologicals in this table have changed. Use 2007 codes on claims through December 31, 2007, and 2008 codes beginning January 1. Drugs marked with an * below are newly added for 2008.
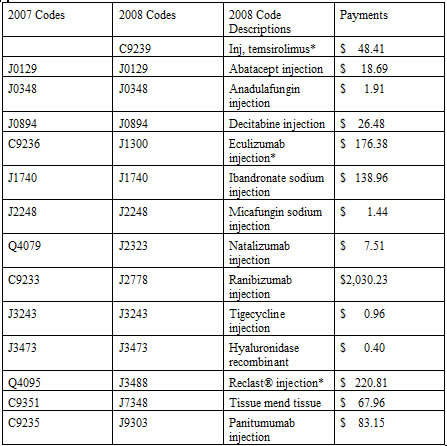
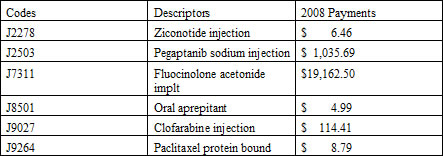
Table 3 includes a list of drugs whose pass-through status will expire on December 31, 2007. These drugs will be reimbursed separately in 2008, but at a rate of ASP + 5 percent.
Table 3: Pass-Through Status Expiring
RPs and Contrast Agents
In 2008, CMS will package all diagnostic radiopharmaceuticals (RPs) and contrast agents with the associated diagnostic test or therapeutic procedure. The agency will base the packaged payment for diagnostic radiopharmaceuticals and contrast agents on average acquisition costs from claims data.
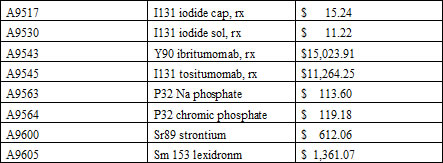
Therapeutic RPs with a median cost per day greater than $60 will continue to receive separate payment in 2008. This payment will be based on average unit costs from 2007 claims data. Table 4 lists all of the 2008 separately payable therapeutic RPs and their final payment rates.
Table 4: Separately Payable Therapeutical RPs
Intravenous Immune Globulin
Current payment for intravenous immune globulin (IVIG) treatments consists of three components:
- Payment for the drug (described by a HCPCS J-code);
- Administration of the IVIG product (described by one or more CPT codes); and
- Preadministration-related services (HCPCS code G0332).
In 2008, CMS will continue payment for preadminstration services, but the code for them (G0332) has been assigned to new clinical APC 0430, which carries an approximate median cost of $37. What that means is that hospitals will receive less for these services, which were previously assigned to new technology APC 1502 with a payment of $71. Payment for pre-administration-related services in a physician's office will remain at $71.
Blood Clotting Factors
CMS proposed providing reimbursement for blood clotting factors at the same rate as other non-pass through, separately payable OPPS drugs. The proposal was finalized. In 2008, blood clotting factors will be reimbursed at a rate of ASP + 5 percent. In addition, the add-on payment (furnishing fee) reimbursed only in physicians' offices will increase to $0.158 per unit administered.
Drug Administration
As you know, last year CMS adopted certain CPT codes and ambulatory payment classifications (APCs) for initial, sequential, and concurrent drug administration services. Medicare will again recognize these codes in the hospital outpatient setting in 2008. However, CMS made final its proposal to not make separate payment for CPT code 90768 (intravenous fusion, for therapy, prophylaxis, or diagnosis [specify drug]), keeping it a packaged service.
Information Source: The final 2008 OPPS rule can be found in the November 27 issue of the Federal Register at http://www.access.gpo.gov/su_docs/fedreg/a071127c.html. Scroll down to Centers for Medicare and Medicaid Services, Rules, Medicare. For section V. OPPS Payment Changes for Drugs, Biologicals and Radiopharmaceuticals, download the PDF version, and go to page 66752.

