Date Posted: Wednesday,
May 05, 2021
The pandemic and the public health emergency (PHE) it brought along with it, have changed how health care is delivered. Commercial payors have been more amenable to paying for telehealth services in prior years. Due to the pandemic, CMS decided to relax its guidelines on telehealth acceptance and payment. More payments equal more scrutiny, though. In this case, that means more involvement from the Department of Homeland Security Office of Inspector General. In order to stay compliant in billing Medicare for the services performed, practices need to understand what the OIG is zoning in on. In this article, the OIG's Work Plan, how it relates to telehealth, and best practices to stay compliant will be discussed.
The Office of Inspector General (OIG)
The OIG was established in 1976 and, via its website, gives the following information:
- Largest inspector general's office in the Federal Government
- Fights waste, fraud, and abuse in Medicare, Medicaid, and over 100 other Department of Health and Human Services (HHS) programs
- Goals and Objectives are to: 1) Fight fraud, waste, and abuse; 2) Promote quality, safety, and value; and 3) Advance excellence and innovation
The OIG is headed by a statutory Inspector Genera that is appointed by the President of the United States and confirmed by the Senate. The Federal Register notes the OIG is comprised of the following six units:
- Immediate Office of the Inspector General. This office consists of the Inspector General, Principal Deputy Inspector General, Chief of Staff, technical advisers, and staff. The Immediate Office makes the contacts with Congress, HHS, the public, and leads congressional, media, and public affairs interaction.
- Office of Management and Policy (OMP). The OMP formulates and executes the OIG's budget, develops policy, manages information technology, human resources, executive resources, procurement activities, and physical space.
- Office of Evaluation and Inspections (OEI). The OEI conducts evaluations of HHS programs, operations, and processes for vulnerabilities and make recommendations for corrective action; prevents and detects fraud and abuse; and promotes efficiency and effectiveness in the HHS programs.
- Office of Counsel to the Inspector General (OCIG). The OCIG provides general counsel and legal advice to OIG.
- Office of Audit Services (OAS). The OAS oversees audits: it establishes audit priorities; performs audits; oversees audit progress; coordinates with other stakeholders; recommends changes to program policies, regulations, and legislation in order to prevent fraud, waste, and abuse, and improve programs and operations; and reports on audit impacts.
- Office of Investigations (OI). The OI takes over if audits lead to investigation by conducting criminal, civil, and administrative investigations of alleged fraud, waste, abuse, mismanagement, and/or violations of the standards of conduct that fall within the jurisdiction of OIG.
The Work Plan
The Work Plan lays out the various projects that are underway or planned by the OAS and OEI. In the past, the Work Plan was updated and published once or twice a year. Consultants, coders, auditors, billers, and others would wait until it was published and go through the latest projects to see what the OIG was concentrating on for the upcoming year. Currently, the OIG updates the Work Plan on its website on a monthly basis.
In choosing projects to add to the Work Plan, the OIG has to look at many things:
- Top challenges facing HHS;
- Work that other organizations are performing;
- Actions taken on previous reviews where OIG made implementation recommendations;
- Mandatory requirements under laws, regulations, and other directives;
- Requests made by Congress, HHS management, or the Office of Management and Budget (OMB); and
- Positive impact potential.
The table below is an example of the recently added items to the Work Plan.
Recently Added Items
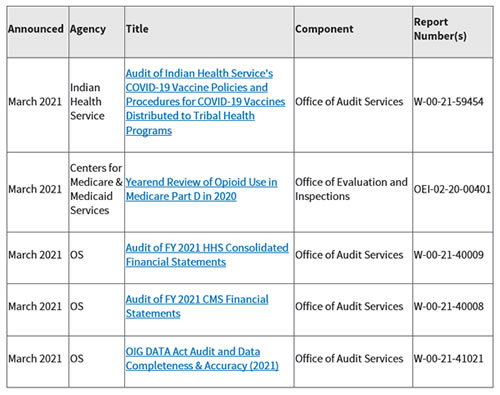
The new items are shown for one month, then moved to the Active Work Plan Items tab. There are also an Archives tab that dates back to 1997.
Why is the OIG Interested in Telehealth?
In April of 2018, the OIG put out a report called, "CMS Paid Practitioners For Telehealth Services That Did Not Meet Medicare Requirements." Obviously from the title, the OIG findings were not favorable; and this was prior to the pandemic. The report states that payments for telehealth services reached over $17 million in 2015, so the OIG wanted to determine if CMS paid properly for telehealth services and that Medicare requirements were being met. A Medicare Payment Advisory Commission (MedPAC) study from 2009 indicated that professional fee claims for telehealth that did not have corresponding originating-site facility fees were most likely paid in error. Next the OIG took over 191,000 claims that were paid for professional fee claims without originating-site fee claims.
From that group, a random sample of 100 claims were reviewed. Following are the specific findings:
- 31 of the 100 claims (31%) that were paid did not meet Medicare requirements
- Of that 31, 24 were unallowable due to the patient being located in a nonrural originating site7 of the 31 claims were billed by institutional providers that were ineligible to bill
- 3 of the 31 claims were provided at unauthorized originating sites
- 1 of the 31 claims was for a noncovered service, and
- 1 of the 31 claims was for a service provided by a physician outside the United States.
The OIG then extrapolated the figures and estimate that Medicare paid for about $3.7 million in improper claims. The OIG made three recommendations from this review: 1) that CMS conduct periodic post-payment reviews to disallow payments for errors that have no telehealth claim edits; 2) that CMS work with the MACs to implement all telehealth claim edits in the Medicare Claims Processing Manual; and 3) that CMS offer education and training sessions regarding telehealth requirements. CMS concurred with all recommendations.
Once the public health emergency (PHE) was declared, CMS began to relax its policies on which telehealth services were allowable in which settings. In February of this year, Deputy Inspector Grimm put out an article stating that the OIG "is conducting significant oversight work assessing telehealth services during the public health emergency…. To help ensure the potential benefits of telehealth are realized for patients, providers, and the HHS programs." These factors have led the OIG to currently have seven (7) different projects running on telehealth based on a variety of different aspects.
The Sweet Seven?
Since it is March Madness time, instead of the Sweet 16, let's talk about the Work Plan's Sweet 7 in relation to telehealth. Of the seven projects, two are related to Home Health, two to Medicaid, with the other three concentrating on various other aspects of telehealth payment.
Let's take a look at each.
Projects that are expected to have reports published in 2021:
- Use of Telehealth to Provide Behavioral Health Services in Medicaid Managed Care. In this project, the OIG is analyzing how behavioral health services are being provided virtually. https://oig.hhs.gov/reports-and-publications/workplan/summary/wp-summary-0000397.asp
- Medicaid: Telehealth Expansion During COVID-19 Emergency. In this project, the OIG is determining if State agencies and providers complied with Federal and State requirements for telehealth services under the national public health emergency declaration. It will also determine if the States gave providers adequate guidance on the requirements for billing telehealth. https://oig.hhs.gov/reports-and-publications/workplan/summary/wp-summary-0000488.asp
- Use of Medicare Telehealth Services During the COVID-19 Emergency. In this project, the OIG is looking at how Medicare beneficiaries are utilizing telehealth compared to the use of in-person services and what types of providers and beneficiaries are offering/using telehealth. https://oig.hhs.gov/reports-and-publications/workplan/summary/wp-summary-0000491.asp
- Medicare Telehealth Services During the COVID-19 Pandemic: Program Integrity Risks. In this project, the OIG is looking at providers' billing patterns and trying to identify the type of providers that may pose a program integrity risk to Medicare. https://oig.hhs.gov/reports-and-publications/workplan/summary/wp-summary-0000535.asp
Projects that are expected to have reports published in 2022:
- Home Health Agencies' (HHA) Challenges and Strategies in Responding to the COVID-19 Pandemic. In this project, the OIG will reveal how HHAs are addressing COVID-19 challenges, like staffing shortages and their emergency preparedness plans. https://oig.hhs.gov/reports-and-publications/workplan/summary/wp-summary-0000557.asp
- Audits of Medicare Part B Telehealth Services During the COVID-19 Public Health Emergency. In this project, the OIG lays out a two-part audit strategy. Phase one audits will look at if E/M services, opioid use disorder, end-stage renal disease, and psychotherapy meet Medicare requirements. Phase two will look at distant and originating site locations, virtual check-ins, electronic visits, remote patient monitoring, use of telehealth technology, and annual wellness visits to see if they meet Medicare requirements. https://oig.hhs.gov/reports-and-publications/workplan/summary/wp-summary-0000556.asp
- Audit of Home Health Services Provided as Telehealth During the COVID-19 Public Health Emergency. In this project, the OIG will review homme health services delivered by HHAs in the PHE to ascertain what types of services are being furnished via telehealth, and if those services are reported according to Medicare requirements. https://oig.hhs.gov/reports-and-publications/workplan/summary/wp-summary-0000553.asp
In considering these projects, it appears that the OIG is more focusing on performance, but, of course, will still suggest Medicare recoup what it considers overpayments.
Telefraud?
The OIG is also making a distinction between "telefraud" and telehealth FRAUD. The phrase telefraud is used to indicate fraud schemes that use telemarketing schemes in conjunction with dishonest physicians performing sham virtual visits. Many times, the physicians are not billing for the telehealth service, but for other services, like durable medical equipment (DME). Be sure to get your phrases correct.
Conclusion
The Work Plan shows that the OIG is looking at many different aspects of telehealth from different types of providers; casting a wide net, so to speak. Take a look through the projects for details on what the OIG is specifically reviewing for each one that pertains to your type of practice/facility. This will then allow internal audits to be set up focused on what the OIG is currently highlighting. This way the practice/clinic/facility can concentrate on the things that are important to the OIG and make sure their documentation of services is in order. Education should be provided to any physicians and other providers that indicate deficiencies. As there are many bills being introduced addressing telehealth post-PHE, it seems that expansion of telehealth services may continue to increase. Keep an eye on Congress so your practice/clinic/facility can ensure compliance with all of the telehealth rules. Stay safe and healthy.
Betty Hovey, CCS-P, CDIP, CPC, COC, CPMA, CPCD, CPB, CPC-I, is the Senior Consultant/Owner of Compliant Health Care Solutions, a medical consulting firm that provides compliant solutions to issues for all types of healthcare entities.
Chcs.consulting

