Date Posted: Tuesday,
November 15, 2016
In our current environment, medical providers are being inundated with demands
from both governmental and commercial payers. With the burden of Comparative
Billing Reports (CBRs), Additional Documentation Requests (ADRs), Pre-payment
Reviews, Post Payment Reviews, audits by ZPICs, MICs, RACs and Commercial
Payers, Denials of medical services for generic reasons such as "Not Medically
Necessary," providers oftentimes find themselves scratching their head asking:
"Is this really worth it?" Articles published in the Wall Street journal
(August 29, 2014), Forbes (September 11, 2014), The Huffington Post (May 30,
2012), Medical Economics (November 21, 2013), and a host of others over the
past 10 years reveal that a very scary percentage of physicians say that,
for a number of reasons, if they had to do it over again, they wouldn't.
And much of the discontent and unhappiness center around what they perceive
as administrative complex and clinically unnecessary rules and regulations.
This is well supported by the fact that there are issues with the contractors
who have been awarded contracts by CMS. To fact check this, you don't have
to go any further than such respected publications such as Forbes and CBS
News. Through investigative reporting, they have seen fit to produce articles
and broadcasts to highlight the issues. In addition, highly respected consultants
have submitted White Papers to the Senate Finance Committee to make their
concerns known. Before I get to the articles and White Paper, let me provide
evidence to confirm that my opinion is grounded in facts and not fairy tales.
1. The Department of Justice obtained more than $3.5 billion in settlements
and judgments from civil cases involving fraud and false claims against the
government in the fiscal year ending Sept. 30, 2015.
a. This is the fourth year in a row that the department has exceeded $3.5
billion in cases under the False Claims Act, and brings total recoveries from
January 2009 to the end of the fiscal year to $26.4 billion.
2. As of June 30, 2016 Strike Force Actions have included :
a. 1,522 Criminal Actions;
b. 2,185 Indictments; and
c. $1.98 billion in recovery
In the van Halem Group, LLC White Paper, item number 2 discusses that one
significant concern is the lack of trust between the provider community and
CMS:
CMS and its contractors often cultivate an environment of mistrust and
suspicion that all providers of certain services are inherently fraudulent.
The sentiment is widely shared by anyone that has worked with CMS contractors
in the area of program integrity and a similar environment is probable within
the CMS Program Integrity Group. This type of environment leads investigators,
contractors, and CMS to pursue providers in an aggressive manner, sometimes
unfairly, based on little evidence or collaboration of any wrongdoing.
The paper goes on to state that they have found that these contractors abuse
the use of prepayment reviews. As an example, "It is not uncommon for a Zone
Program Integrity Contractor (ZPIC) to implement a 100% prepayment review
of a provider's claims with no notification."
Simply making a statement that payers and their "Contracted Bounty Hunters"
are on a "Rampage" (Narratives provided by CBS News and Forbes) (*specific
links to these stories are provided above) is a statement most would look
at and think, "Well, sure they're aggressive," but until you see it in the
terms of actual pre- and post-payment reviews, the magnitude of the problems
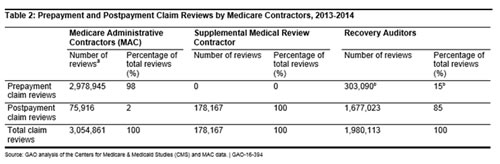
remain nuanced. The table below only takes into account MACs, SMRCs and RACs.
ZPICs, MICS, Commercial Payers, etc. are not included.
In 2015, the OIG was very critical of the Centers for Medicare and Medicaid
Services regarding the award of ZPIC Contracts and the lack of oversight for
these contractors. According to the OIG Report of the same year:
The Centers for Medicare & Medicaid Services requires potential Medicare
antifraud contractors to disclose possible conflicts of interest and strategies
for mitigating them (This information is published in multiple public reports).
But when officials from the Department of Health and Human Services Office
of Inspector General reviewed these disclosures, they identified 1,919 business
and contractual relationships as possible conflicts and 16 as actual conflicts,
according to the report. In their review, OIG investigators looked at information
from 18 offerors (companies that put in proposals for contracts) and 85 subcontractors
within CMS...Often the ZPIC contractors have had no experience in the areas
of fraud and abuse for which they should be accountable. The result is a loss
to CMS of fraud and abuse funds and providers, many of which are small – medium
sized businesses, are forced to spend thousands of dollars to address unfounded
audits and investigations. This was evidenced when CMS lost $80 million of
the $120 million paid to contractors in 2011, due to poor data when investigating
fraud and abuse...The significant lack of oversight of ZPIC contractors, who
were awarded contracts averaging $81.9 million, is evidenced by the extreme
and ill-founded actions taken by some ZPICs in unwarranted efforts to show
CMS a return on investment. Contractors often employed significant, aggressive,
and over-zealous audits, claims reviews and investigations against legitimate,
not fraudulent, providers of healthcare services. The broad brush actions
cost legitimate providers huge amounts of time, money and energy-inhibiting
their ability to provide care to beneficiaries. Some are forced to leave Medicare,
if not health care services all together. ZPICs are large and powerful corporations
with the backing of the federal government. They apply heavy handed processes
in a punitive manner to many legitimate providers over minor document infractions.
Further exacerbating the problems are the individuals employed by CMS to oversee
these contractors, who are often young and inexperienced and do not have healthcare
or fraud investigation experience.
For a couple of years now, I have talked about The Treating Physician Rule.
The first section of the Medicare statute is the prohibition "Nothing in this
title shall be construed to authorize any Federal officer or employee to exercise
any supervision or control over the practice of medicine or the manner in
which medical services are provided." From this, one could conclude that
the beneficiary's physician should decide what services are medically necessary
for the beneficiary, and a substantial line of authority in the Social Security
disability benefits area holds that the treating physician's opinion is entitled
to special weight and is binding upon the Secretary when not contradicted
by substantial evidence. Some courts have applied the rationale of the "treating
physician" rule in Medicare cases, and have rejected the Secretary's assertion
that the treating physician rule should not be applied to Medicare determinations.
In Holland v Sullivan, the court concluded:
Though the considerations bearing on the weight to be accorded a treating
physician's opinion are not necessarily identical in the disability and Medicare
context, we would expect the Secretary to place significant reliance on the
informed opinion of a treating physician and either to apply the treating
physician rule, with its component of "some extra weight" to be accorded that
opinion, [even if contradicted by substantial evidence], or to supply a reasoned
basis, in conformity with statutory purposes, for declining to do so.
In addition, audit findings may be challenged based upon the opinion of the
treating physician who is likely the target of the audit. The "Treating Physician
Rule" first arose in a context of a disability determination and holds that
an Administrative Law Judge should give greater deference to the opinion of
the treating physician than to those of non-treating physicians. The opinion
of the treating physician is particularly important when challenging the applicability
or reasonableness of a LCD.
The Van Halem Group's White Paper to the Senate Finance Committee outlined
and focused on the clinical competency of those both clinically and non-clinicians
making determinations on "Medical Necessity." Until June of 2011, CMS Section
3.4.5.C of the Medicare program Integrity Manual (Pub 100-8) guided contractors
in performing complex medical reviews.
While Medical Review (MR) staff must follow national coverage determinations
and local coverage determinations, they are expected to use their expertise
to make clinical judgments when making medical review determinations. They
must take into consideration the clinical condition of the beneficiary as
indicated by the beneficiary's diagnosis and medical history when making these
determinations. Currently, ZPIC and Medicare Administrative Contractors (MACs)
are employing clinical staff; however, they have no ability to use that expertise.
As a result, CMS is requiring and paying for clinical expertise but not receiving
the cost savings benefit of the expertise. Additionally, a provider under
review may be subject to significant claim denials and scrutiny because of
issues with insufficient documentation that are not associated with fraudulent
activity. Many denials are unfounded and irrational due to the prohibition
of allowing ZPIC's clinical staff to use their clinical judgment and expertise.
As a result, these denied claims must be appealed, often times up to the Administrative
Law Judge (ALJ) level. This process of denying claims and conducting appeals
costs the government a significant amount of money only to see a significant
number of the decisions overturned.
While medical providers are held to very strict standards with regard to documentation
and coding of services, the payers aren't, and this oftentimes leads to unethical
business practices. Take for instance the Medicare Appeals Process. After
exhausting the first 2-levels of the process (Redetermination and Reconsideration),
a practice has the right to file for an Administrative Law Judge Hearing,
which according to CMS Section 1869 of the Social Security Act and 42 C.F.R.
part 405 subpart I, OMHA ALJs began adjudicating appeals in July 2005, based
on section 931 of the MMA, which required the transfer of responsibility for
the ALJ hearing level of the Medicare claim and entitlement appeals process
from SSA to HHS. New rules at 42 CFR part 405, subpart I and subpart J were
also established to implement statutory changes to the Medicare fee-for-service
(Part A and Part B) appeals process made by the Benefits Improvement Protection
Act (BIPA) in 2000 and the Medicare Modernization Act (MMA) in 2003. Among
other things, these new rules addressed appeals of reconsiderations made by
QICs, which were created by BIPA for the Part A and Part B programs. These
rules also apply to appeals of SSA reconsiderations. The statutory changes
made by BIPA include a 90-day adjudication time frame for ALJs to adjudicate
appeals of QIC reconsideration beginning on the date that a request for an
ALJ hearing is timely filed.
In recent years, the Medicare appeals process has experienced an unprecedented
and sustained increase in the number of appeals. At OMHA, for example, the
number of requests for an ALJ hearing or review increased 1,222 percent, from
fiscal year (FY) 2009 through FY 2014. The increasing number of requests has
strained OMHA's available resources and resulted in delays for appellants
to obtain hearings and decisions. Right now, it is taking between 2-3 years
to have a case assigned to a judge and then up to another 2-3 years to have
the case heard. The biggest issue is what happens following a Qualified Independent
Contractor (QIC's) decision to uphold a redetermination, finding Medicare
has the right to demand a refund or to begin off-setting monies from future
payments. They can do this even though "due process" has not been granted
to the appellant, resulting in a finding of "guilty" by a non-binding entity
such as a contractor. These financial losses are crippling medical practices
and forcing them into uncharted waters of having to provide services for Medicare
beneficiaries without being compensated, because someone other than a judge
made a decision that their services billed were not "Medically Necessary"
or failed to support the level billed, which we all know is highly subjective.
Despite significant gains in OMHA ALJ productivity (in FY 2014, each OMHA
ALJ issued, on average, a record 1,048 decisions and an additional 456 dismissals),
and CMS and OMHA initiatives to address the increasing number of appeals,
the number of requests for an ALJ hearing and requests for reviews of QIC
and IRE dismissals continue to exceed OMHA's capacity to adjudicate the requests.
As of April 30, 2016, OMHA had over 750,000 pending appeals, while OMHA's
adjudication capacity was 77,000 appeals per year, with an additional adjudication
capacity of 15,000 appeals per year expected by the end of Fiscal Year 2016.
If this is not a sign of payers on an auditing rampage, then I am not sure
what would constitute one. In general, payers are asking physicians to provide
first-world care in the presence of third-world due process.
One of the topics I discuss during calls with clients who have been targeted
or have received adverse results from an audit or during lectures is that
they have a right to "Challenge Credentials of Reviewers." Specifically, Section
3.1.1.1 of the Medicare Integrity Manual requires that coverage determinations
be made only by RNs, LPNs, or physicians, unless the task can be delegated
to another licensed health care professional. Reviews of coding determinations,
likewise, must be made by certified coders, but should also be made by those
who possess the requisite skills in the specialty they are reviewing. Upon
receipt of disclosure of the identity and qualifications of the auditors,
request for the disclosure of the identity and qualifications of the auditors
should be made. Should the matter be escalated to an ALJ hearing, you have
the right to request formal discovery of such materials.
The van Halem Group's paper outlined the fact that "There is a lack of experience
and training of ZPIC staff." In one specific case, a member of management
at a ZPIC was questioned regarding issues surrounding numerous errors being
made by staff. The ZPIC Manager said, "Not only was he aware of the errors
being made but attributed them to issues related to workload, exhaustion,
or lack or training." The White Paper goes on to state, "Many ZPIC investigators
lack sufficient training in coverage and reimbursement policies for the services
under their review." There was a case sited in the paper where a provider
contacted their local Congressman to address concerns over incorrect denials
in a ZPIC audit. The Congressman's office contacted CMS Central Office and
submitted 11 examples of claims denied in error. The actual written response
from CMS said they agreed that 7 of the 11 claims were in fact denied erroneously.
However, the letter went on to state, "That regardless, the provider's error
rate remained high so they will remain under investigation" despite the fact
they had just received confirmation in the very same response that the error
rate calculated was incorrect because of errors made by the contractor. This
not only supports a lack of training, but a lack of appropriate oversight
and fairness."
One of the areas our firm focuses on, specifically through Frank Cohen, is
challenging the sampling and extrapolation of an audit finding. The statutory
or regulatory provision expressly authorizes the use of extrapolation. However,
"... sample adjudication represents a judicially approved procedure that can
be reconciled with existing Medicare requirements for case-by-case considering..."
Case law clearly holds that a presumption of validity attaches to the amount
of an overpayment. Thus, the burden of proof with respect to a challenge
to the statistical validity of an extrapolated demand rests squarely with
the provider. 42 U.S.C. § 1395-ddd holds that a Medicare contractor may not
use extrapolation to determine overpayment amounts absent a determination
that there is a "sustained high level of payment error or documented educational
intervention has failed to correct the payment error." Such determinations
may be made by a variety of methods including a PROBE sample or data analysis
and are not subject to administrative or judicial review. In Gentiva Health
Care Corp. v. Sebelius, 857 F.2d 1 (D.D.C. 2012), the court held that the
responsibility for determining the existence of sustained high level of payment
error or the failure of educational intervention may be delegated to contractors.
Thus, the threshold for determining whether an extrapolated demand may be
made rests with the contractor and is largely immune from review. The propriety
of demand based upon a statistically valid random sampling is well-settled
and the premise is not subject to challenge.
According to Frank Cohen, this does not, however, preclude contractors from
the responsibility to generally accepted statistical standards and guidelines.
Section 4.2 of Chapter 8 of the CMS Program Integrity Manual states the following:
"If a particular probability sample design is properly executed, i.e., defining
the universe, the frame, the sampling units, using proper randomization, accurately
measuring the variables of interest, and using the correct formulas for estimation,
then assertions that the sample and its resulting estimates are ‘not statistically
valid' cannot legitimately be made."
Cohen asserts that first of all:
That is simply a ridiculous statement; of course there are additional
reasons that one could opine that a sample is ‘not statistically valid.'
But within that paragraph, the PIM does outline six specific conditions that
must exist in order for a sample to be considered acceptable. It is simply
not enough for a sample to be just random. It is well established within
the statistical community that a random sample of a heterogeneous universe
rarely produces an appropriate sample for extrapolation. In order for the
sample to be considered as part of an extrapolation event, the sample must
be representative of the universe to which the sample results will be inferred.
This is not just statistically correct; it also concurs with good sense.
It is simply illogical to attempt to take the results of a sample that does
not statistically represent the universe and then try to extrapolate back
to that universe for the purpose of estimating the impact of those erroneous
results.
Yet, this is what happens more often than not and as a result, extrapolations
are overturned at the ALJ level at a very high rate. And when that happens,
the contractor will often appeal this to the MAC, who ends up sending it back
down to the ALJ for reconsideration. Quite often, contractors will quote
Chaves to support that the only requirement is that the sample is random,
yet that is not what the judge said:
Absent an explicit provision in the statute that requires individualized
claims adjudications for overpayment assessments against providers, the private
interest at stake is easily outweighed by the government interest in minimizing
administrative burdens; in light of the fairly low risk of error, so long
as the extrapolation is made from a representative sample and is statistically
significant, the government interest predominates. (Emphasis added.)
My job is that of a physician advocate. My assignment is to protect my
clients from what I (and they) see as unwarranted attacks on their work and
profession. I have been doing this for a long time (21 years to be exact)
and in the overwhelming number of cases, my physician clients are honest,
hard-working, competent, and caring professionals. Most came into medicine
with a single goal: to be paid reasonably for providing quality care to their
patients. At times, it feels like payers have the opposite goal: to not pay
them reasonably for providing quality care to their subscribers. Most providers
with whom I work live in the stress that sometime in the future, some payer
is going to demand that the provider repay them for some service that was
provided maybe three or four years earlier. That's plain insanity.
I don't have expectations that things will change in the near future. In
fact, along with many other well respected experts in this industry, I expect
it to continue to get worse for healthcare providers.
Sean M. Weiss, CMCO, CMPA, CPC-P, CPC, Partner/ Vice President of
Compliance, DoctorsManagement
With Contributions by: Frank Cohen, Director of Analytics and Business Intelligence
Since 1956, DoctorsManagement, a medical and health care consulting firm,
has helped physicians in all specialties with health care, dental and medical
practice management services in virtually every state across America. With
our health care and medical consulting firm’s help, you become free
to concentrate on your life's work AND your life outside of work, as well.
http://www.doctors-management.com/

